Powering Value-Based Care Programs for Pharmacies and Payers
Powering Value-Based Care Programs for Pharmacies and Payers


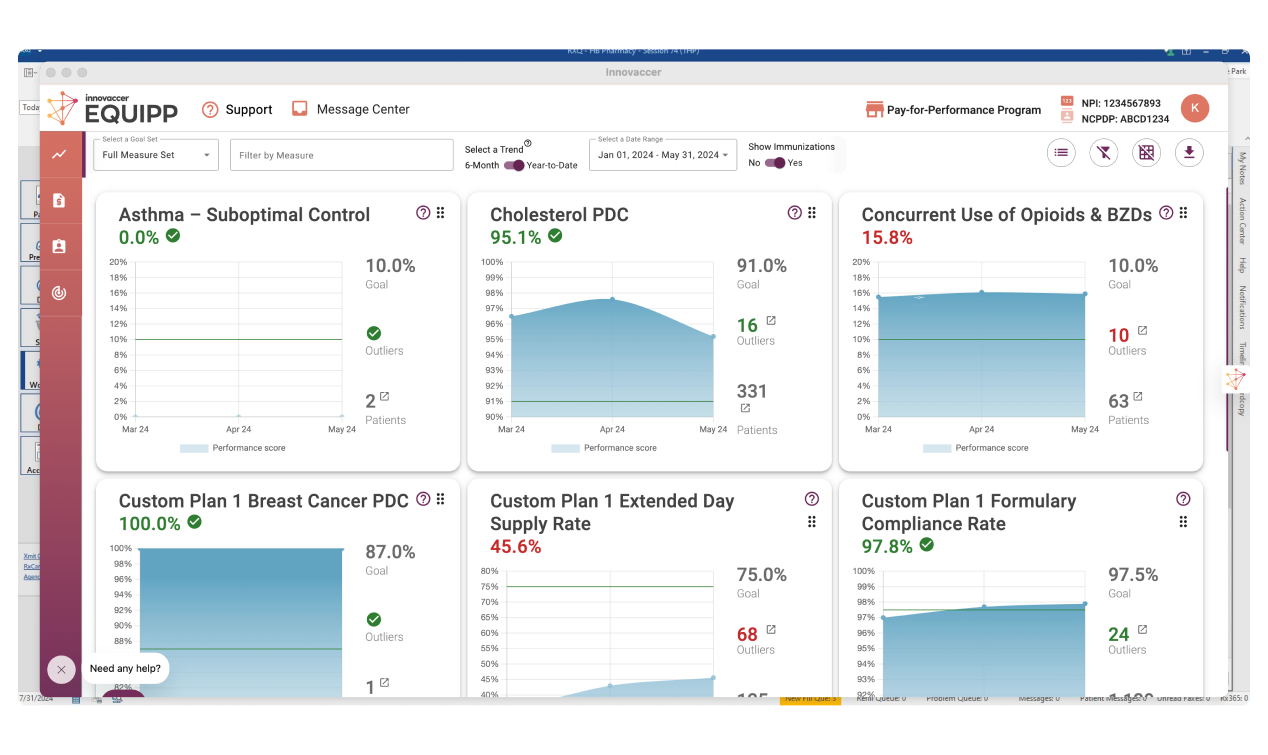
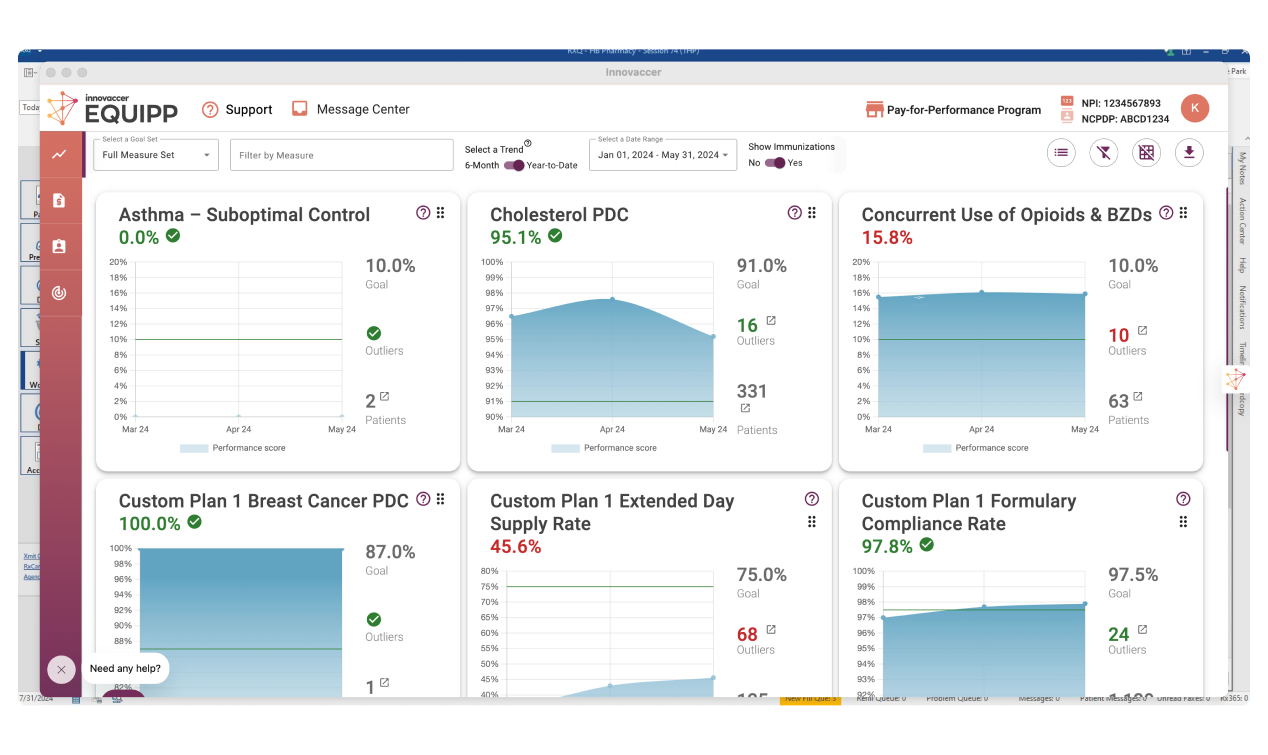
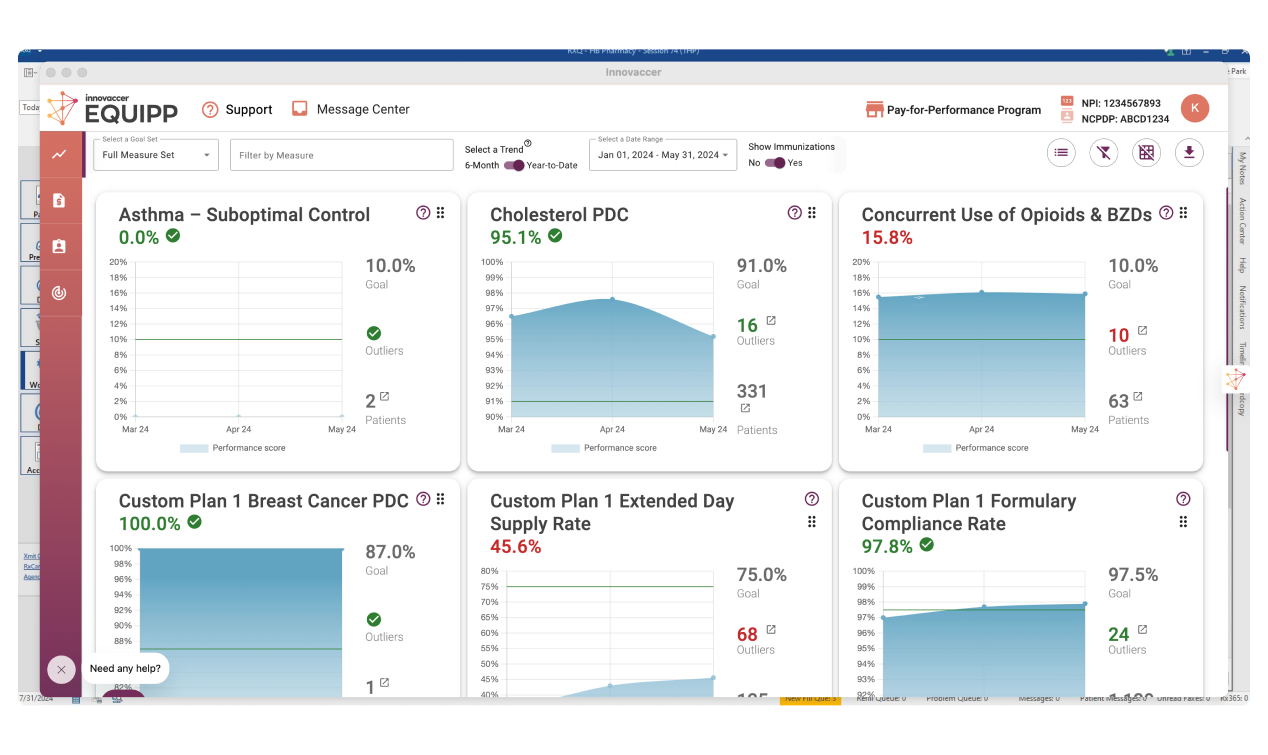




YOY increase in statin adherence
YOY increase in diabetes adherence

pharmacy network coverage
direct impact on HEDIS® numerators


pharmacies actively participating
YOY increase in RASA adherence