Quality Management
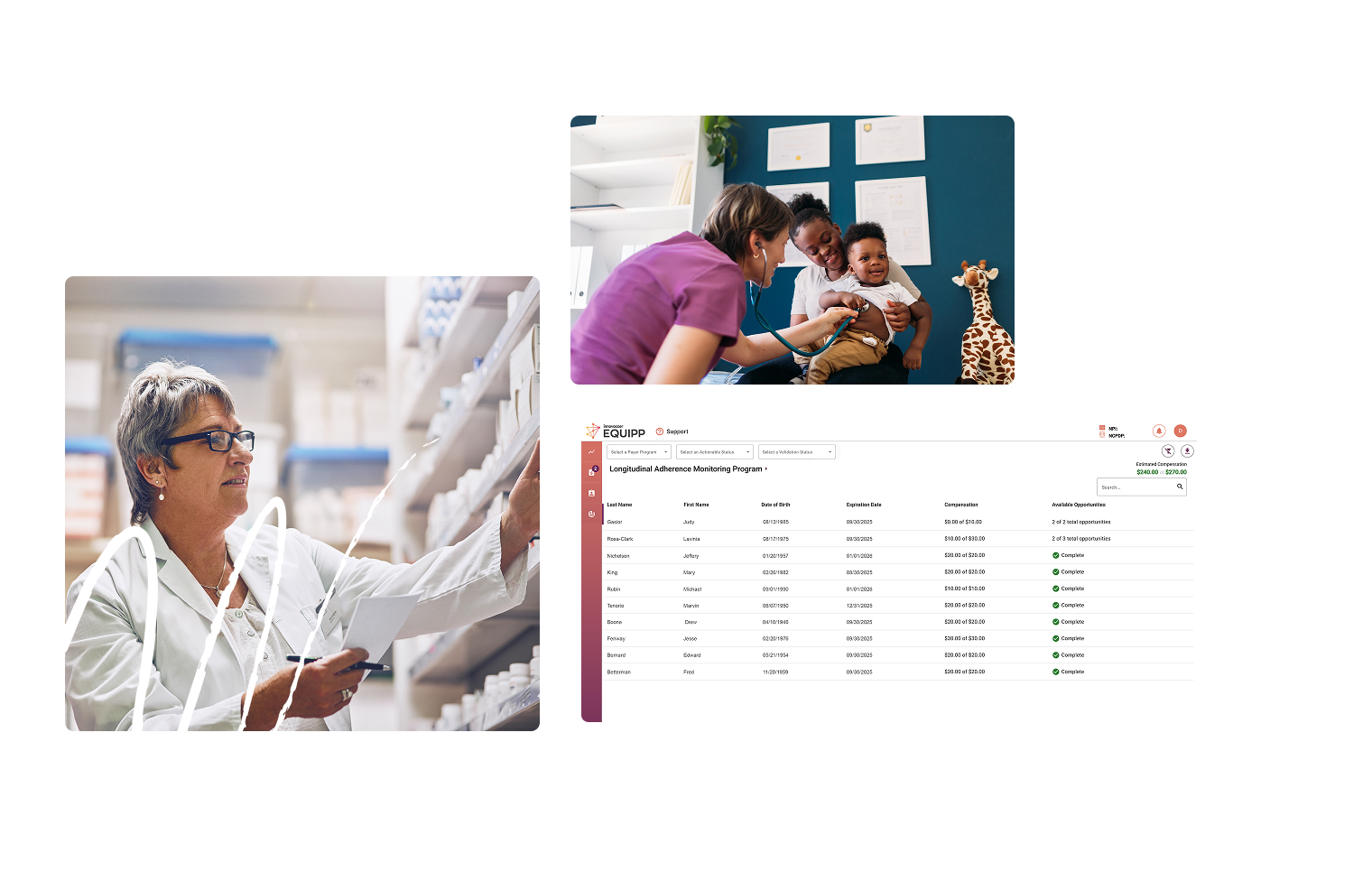
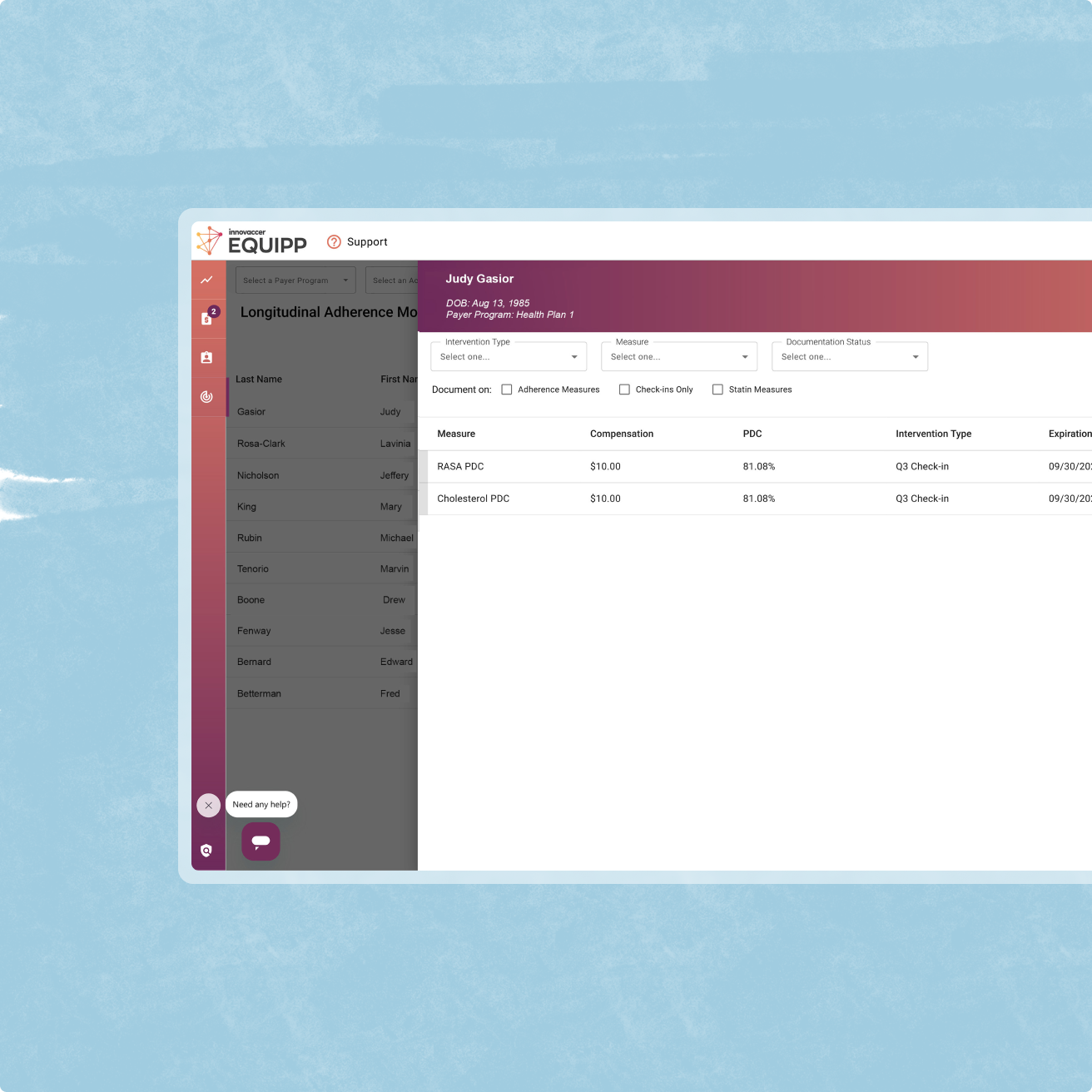
Boost PQA/NCQA quality measures with pharmacy-powered solutions that work. PQS's Quality Management solutions connects health plans with community pharmacies to improve medication adherence, preventive care, and key performance metrics through our industry-leading EQUIPP® platform.
Streamlined pharmacy workflows, performance tracking and incentives, and proven programs like LAMP adherence monitoring and immunization initiatives can result in higher adherence rates, improved preventive care, and valuable point-of-care data collection.
Streamlined pharmacy workflows, performance tracking and incentives, and proven programs like LAMP adherence monitoring and immunization initiatives can result in higher adherence rates, improved preventive care, and valuable point-of-care data collection.
.png)


.png)
.svg)
.png)
.svg)
.png)
.svg)








.png)

.png)

.png)
.png)

.png)