EQUIPP® enables care at scale,
provides data and actionable insights
Using the EQUIPP technology platform, we develop and streamline care opportunities from multiple payer sponsors to send to our pharmacy partner network.
EQUIPP fuels patient-level care with measurable results
Pharmacy’s go-to source for data-driven interventions, benchmarked data and insights. With industry-wide adoption, EQUIPP helps pharmacies deliver care and see measurable results.

The EQUIPP Advantage
We simplify healthcare data, analysis, and reporting
After managing data for 60 million lives, we developed a proprietary process to ingest fragmented data, apply powerful analytics to identify patients, and prioritize care that maximizes impact.
PUT EQUIPP TO WORK
Consolidate fragmented data
Payer provides member eligibility data, pharmacy and medical claims.
PQS ingests, standardizes, and transforms data enabling transparency.
Simplify complex analysis
Calculate quality measures to measure stewards’ specifications.
Powerful analytics identify and prioritize member-level opportunities for quality improvement.
Manage performance with EQUIPP
Adopted industry-wide, EQUIPP displays patient-level care opportunities, benchmarked data, and insights.
Deliver patient care through pharmacies
Patients receive personal care near home with consults on adherence, patient safety, and more
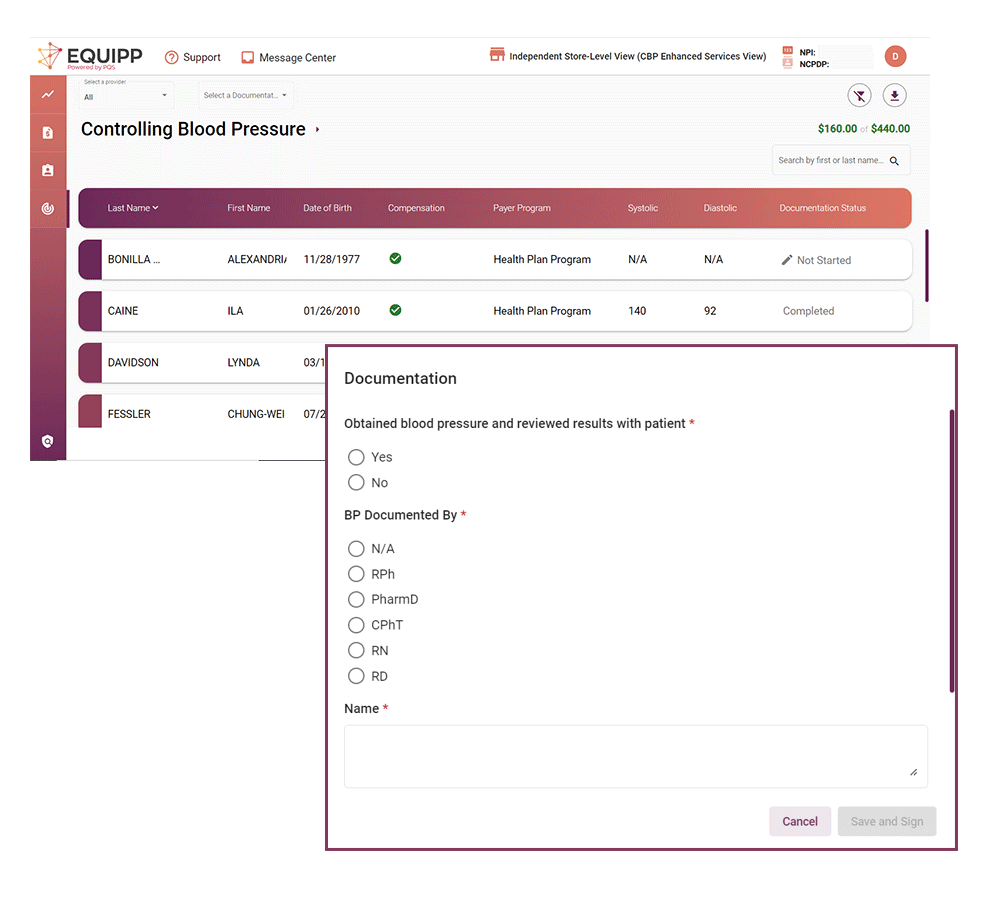
Pharmacies capture clinical data to monitor treatment goals for blood pressure, diabetes A1c, and more.
Bi-directional clinical
data exchange
Support pharmacy collection of patient data back to payers
Create supplemental HEDIS® data files.
See measureable
results
Manage pharmacy services delivery, find actionable insights, and optimize performance.
EQUIPP’s re-architected platform makes it easier for pharmacies to deliver patient care.
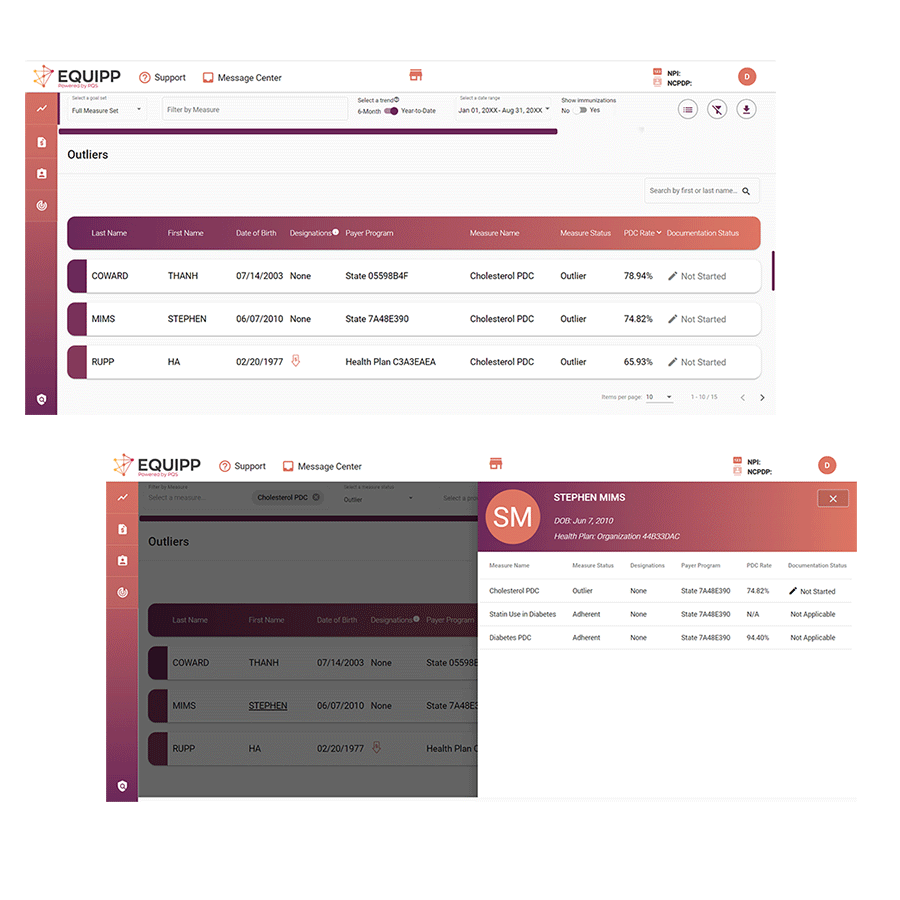
Quickly access patient opportunities on the dashboard
Simplify care with patient details for each measure – all on one screen
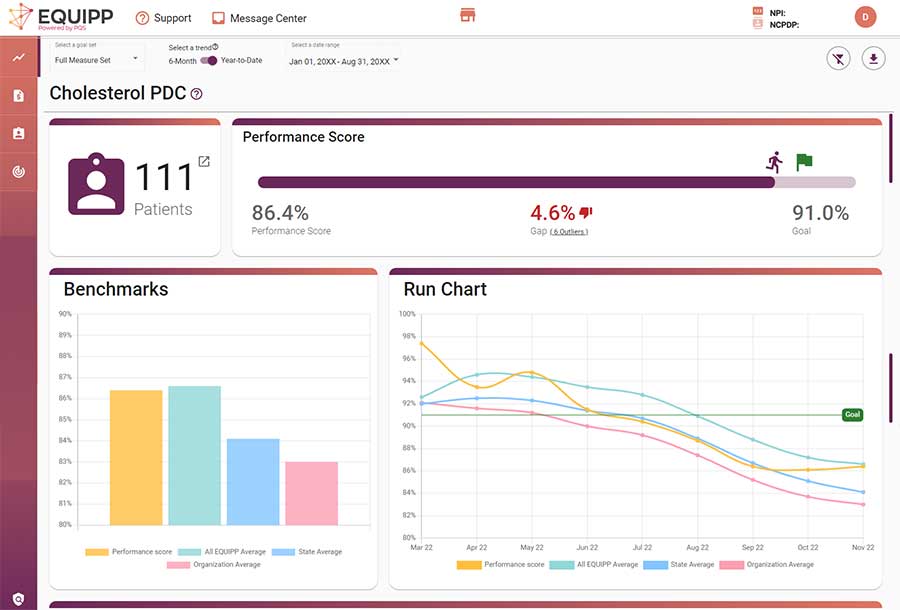
Measure program performance and compare vs. benchmarks on the measure screen
Improve health outcomes for targeted member populations with the Gap Closure Program
Support and resources
for improvement
Tap our expertise to improve patient and
business outcomes
With 10+ years of quality measurement expertise and deep pharmacy knowledge, PQS provides best-practices to develop innovative quality strategies to support more effective interventions.
10+ Years
of quality experience